Where Revenue is Lost
Recently, I was asked by a doctor working in the public system why I thought employees in public hospitals needed to know about billing. His impression was that billing was “not their job” and had no impact on their income.
This question highlights two critical issues at the heart of private patient billing:
❌ Knowledge Gap – Many doctors do not understand how private patient revenue directly links to their own salary through Right of Private Practice (RPP) arrangements, while also reducing salary costs for Local Health Districts (LHDs).
❌ Risk Gap – Many also do not recognise that they are ultimately responsible for ensuring all billing is full, accurate, medically valid and justified. Even if the billing department processes the claim, doctors remain (at least in part) liable for errors.
This knowledge gap and risk exposure form the backdrop to why private patient billing in public hospitals must be seen as everyone’s business.
Want to learn more about the Hospital Billing Chain? Listen to our presentation here.
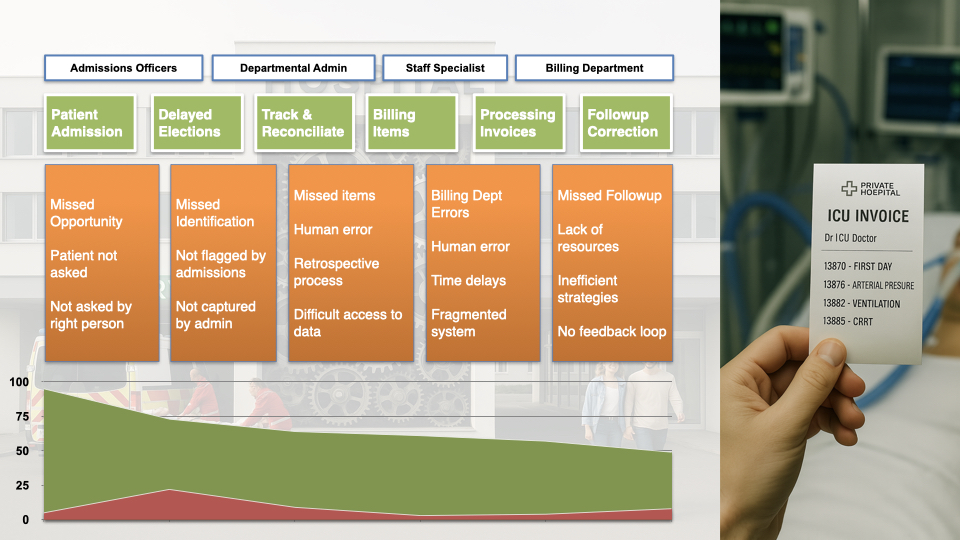
The Billing Chain – Six Key Risk Points
1. Patient Admission and Election
❌ Risk: Critically unwell patients, inter-hospital transfers, and emergency admissions are often not interviewed at admission. When untrained staff handle these conversations, or when no KPI exists to ensure 100% of patients are offered the possibility of private election, revenue is lost immediately.
✅ Solution: Dedicated admissions officers trained in private election conversations, supported by KPIs to ensure complete capture.
2. Deferred or Missed Elections
❌ Risk: Patients who cannot elect at admission are rarely followed up or tracked after ICU discharge. Election changes are not communicated, and many eligible patients are lost entirely.
✅ Solution: A robust tracking system for unelected patients, with follow-up workflows post-discharge.
3. Generating Billing Sheets
❌ Risk: Billing sheets for long admissions, in particular ones that involve transfers between units often either miss days or contain overlaps that lead to double billing and rejections.
✅ Solution: Dedicated clerical support, standardised templates, and clear accountability for billing sheet accuracy and reconciliation.

4. Entering Billing Items
❌ Risk: Human error, retrospective documentation, and lack of EMR integration mean key services such as ultrasound, transfusions, and procedures are consistently under-recorded. We estimate 5–10% of billable value is lost here and one representative audit found 60% of billing sheets contained omissions or errors.
✅ Solution: EMR–billing software integration to reduce transcription, coupled with clinician education on item capture.
5. Submitting and Processing Invoices
❌ Risk: Typos, delays, duplicate entries, and paper-to-electronic conversion errors result in significant rejection rates. Audit data revealed the large majority of non-zero balance invoices are in fact theoretically recoverable errors:
- 15% clerical error requiring correction and resubmission
- 63% unpaid invoices requiring insurer follow-up (often OSHC/OVHC)
- 16% ECLIPSE rejections requiring resubmission
Only a small percentage of outstanding invoices had to be written off – largely made up of claims for ineligible overseas visitors with no insurance.
✅ Solution: Digital-first workflows and automated error checks before submission.
6. Follow-up of Rejections
❌ Risk: Overseas visitors, students, and complex claims often require resource-intensive followup. Without a feedback loop, many legitimate claims are abandoned. Workforce shortages and limited resources mean high value invoices are given priority and low value claims often never get chased.
✅ Solution: Dedicated rejection management teams with defined escalation pathways.
Why Private Patient Billing Matters
For doctors in NSW, captured billings determine access to their full Right of Private Practice (RPP) allowance. Every missed claim directly reduces their remuneration.
At the same time, higher RPP levels reduce salary costs for the LHD. Every unbilled service is not only lost income — it is also a lost cost saving for the system.
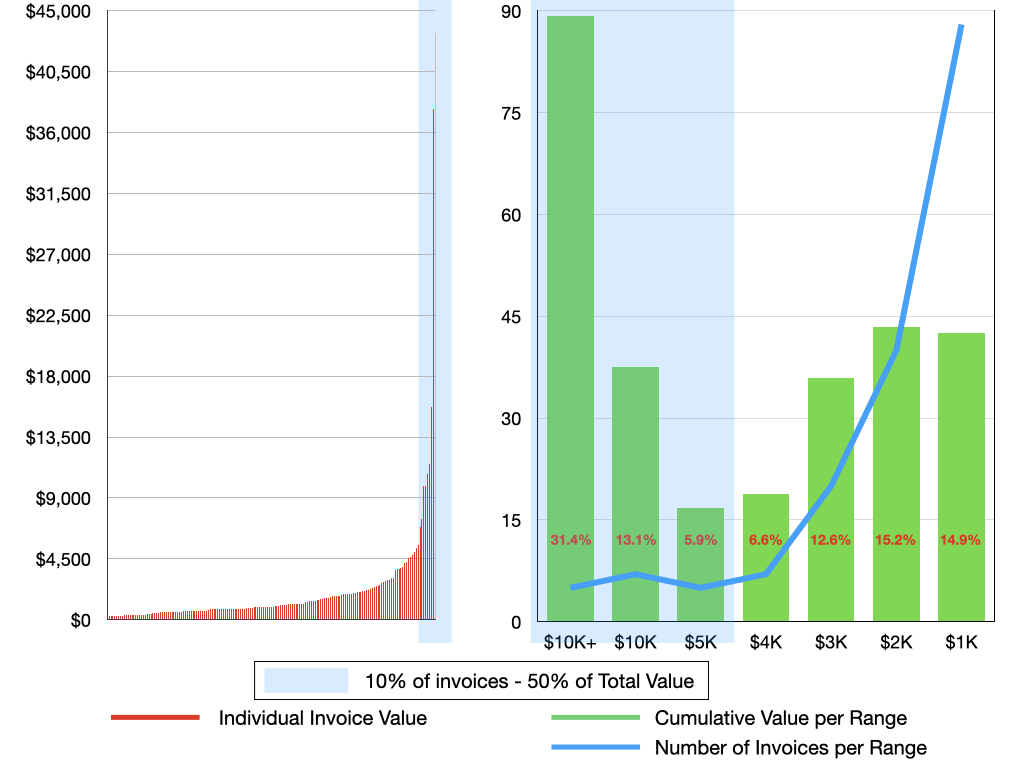
Case Study – ICU Billing Audit Findings
A recently performed ICU audit illustrates the true financial cost:
- ❌ Items Missed by Doctors – 5–10% of billable value lost through incomplete item capture and clerical error.
- ❌ Unpaid Invoices and Processing Errors – 15% clerical error, 16% rejection required resubmittion, 63% required insurer follow-up.
- ❌ Missed or Incomplete Billing – Over 30% of billable patients were incompletely billed or missed entirely.
Why Missing Patients Matters
When we break down the data, most missed invoices are small in value — less than $1,000 each. However, the small minority of high-value admissions, where invoices reach into the thousands or tens of thousands of dollars, account for more than half of all lost revenue. This means that even a single missed patient can have a significant financial impact. In other words: we cannot afford to miss even one patient.
Towards a Zero Margin Policy
The data is clear: every single billable patient must be billed, every single time. Achieving this requires a zero margin policy, with:
✅ Education – Clinicians trained in claim rules and item interactions.
✅ Clerical Support – Dedicated secretarial staff producing accurate billing sheets.
✅ IT Solutions – EMR–billing software integration to minimise manual transcription.
✅ Audit and Feedback – Continuous monitoring to detect and correct systemic errors.
✅ Clear Responsibilities – Defined roles for admissions, clinical, clerical, and billing staff.
Conclusion
Small inefficiencies — a missed interview, an incomplete billing sheet, or a rejected invoice not resubmitted — may look minor in isolation. But across hundreds of admissions, the cumulative effect is staggering.
For both clinicians and hospitals, the reality is unavoidable: a zero margin policy is not aspirational — it is essential.
How ClaimLogic Can Help
At ClaimLogic, we support ICUs and public hospitals to achieve a zero margin policy in practice.
We can assist at every stage of the billing process, from:
- ✅ Comprehensive audits that uncover issues you may not even be aware of
- ✅ Workflow design to strengthen weak points in the billing chain
- ✅ Potential IT integration solutions to bridge gaps between EMRs and billing systems
Most importantly, we don’t just identify problems — we provide workable solutions that are guaranteed to generate tangible results.
Let us help you stop losing revenue.
Get in touch today, and together, we’ll fix the gaps, strengthen your hospital’s billing system, and make sure no patient, no service, and no billable item is ever missed.
Disclaimer
This blog is provided for educational and general informational purposes only and does not constitute legal, medical, or financial advice. While every effort has been made to ensure accuracy, billing requirements under the Medicare Benefits Schedule (MBS) are complex and subject to change. Clinicians should always consult the official MBS, relevant hospital policies, or seek independent professional advice before making billing decisions. While we use reasonable effort to ensure that our overview articles are accurate, current and complete, we do not represent, warrant, or guarantee (to the maximum extent permitted by law) their accuracy, currency, or completeness or imply that they are applicable to your individual situation. ClaimLogic accepts no liability arising from for actions taken based on the content of this article.


